Endometriosis
What is endometriosis?
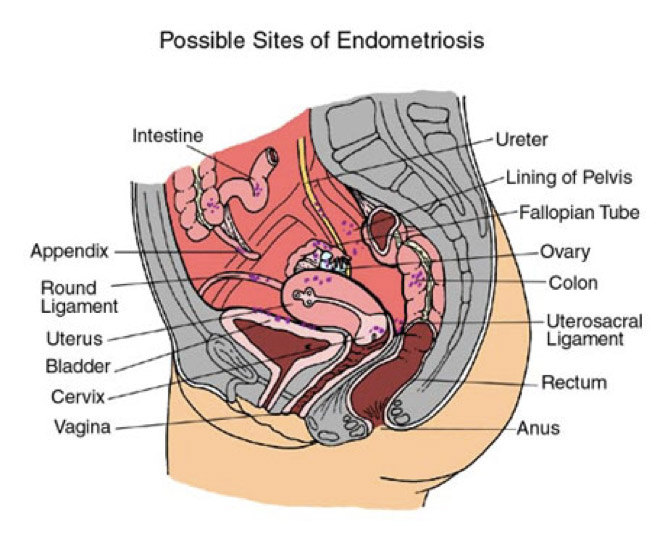
Endometriosis develops when endometrial implants, comprised of tissue normally found within the uterus, are present in other areas of the body, most commonly, inside the abdominal cavity (belly). As this tissue continues to thicken, break down, and bleed during the menstrual cycle (as it happens with the endometrium- inside lining of the uterus), it becomes trapped within the body. Scar tissue and adhesions form, and this can cause organ fusion, anatomical changes and consequently, chronic pelvic pain and infertility.
Endometriosis affects around at least 15% of women in reproductive age. The percentage is even higher in infertile women.
Which are the symptoms?
Because of the difficulty in the diagnosis, there is a delay of about 7 years to make the diagnosis in the United States.
The following are the most common signs and symptoms of endometriosis:
- Painful periods (dysmenorrhea): Pelvic pain and cramping may begin before your period and extend several days into your period. You may also have lower back and abdominal pain.
- Pain with intercourse (dyspareunea): Pain during or after sex is common with endometriosis.
- Pain with bowel movements (dyschezia) or urination (dysuria), usually, during your period.
- Excessive bleeding: You may experience occasional heavy periods (menorrhagia) or bleeding between periods (menometrorrhagia).
- Infertility: Endometriosis is first diagnosed in some women who are seeking treatment for infertility.
- Other symptoms: You may also experience fatigue, diarrhea, constipation, bloating or nausea, especially during menstrual periods.
The severity of your pain isn't necessarily a reliable indicator of the extent of the disease. Some women with mild endometriosis may have intense pain, while others with advanced endometriosis may have little pain or even no pain at all.
Book your consultation
Consultation in person - X-Clinic
Av. Eng. Duarte Pacheco, nº26 - Piso intermédio 1070-110 Lisboa (in fronte of Amoreiras Shopping)
Consultation in person - Medmulher
Av. Marquês de Tomar 44 1050-162 Lisboa
Online/Video Consultation
Zoom meeting
Contact us:
